Healthcare Management Analytics
Providing actionable insights
Good data drives good decisions. No where is that truth more consequential than in the domain of healthcare. Yet, in spite of the billions of GB of data that our healthcare system routinely collects, only a tiny fraction is utilized in a constructive manner that helps diagnosis, treatment, and care management.
The sheer volume of data totally overwhelms the human capacity to spend screen time viewing, organizing, analyzing, and applying to healthcare decision-making. In stark contrast to expedited lab results and diagnostic study reports and on-site, 24/7 clinical monitoring in hospital settings, the vast majority of subacute, post-acute, and chronic care management takes place outside the institutional walls of healthcare, mostly in the home. This poses significant challenges and the potential for gaps in care continuity, as well as issues with timely communication and access to advice or urgent intervention.
Enter Artificial Intelligence...BettrAi has aptly identified and captured the phenomenal leaps forward that are made possible by integrating AI analytics into the process of managing healthcare.
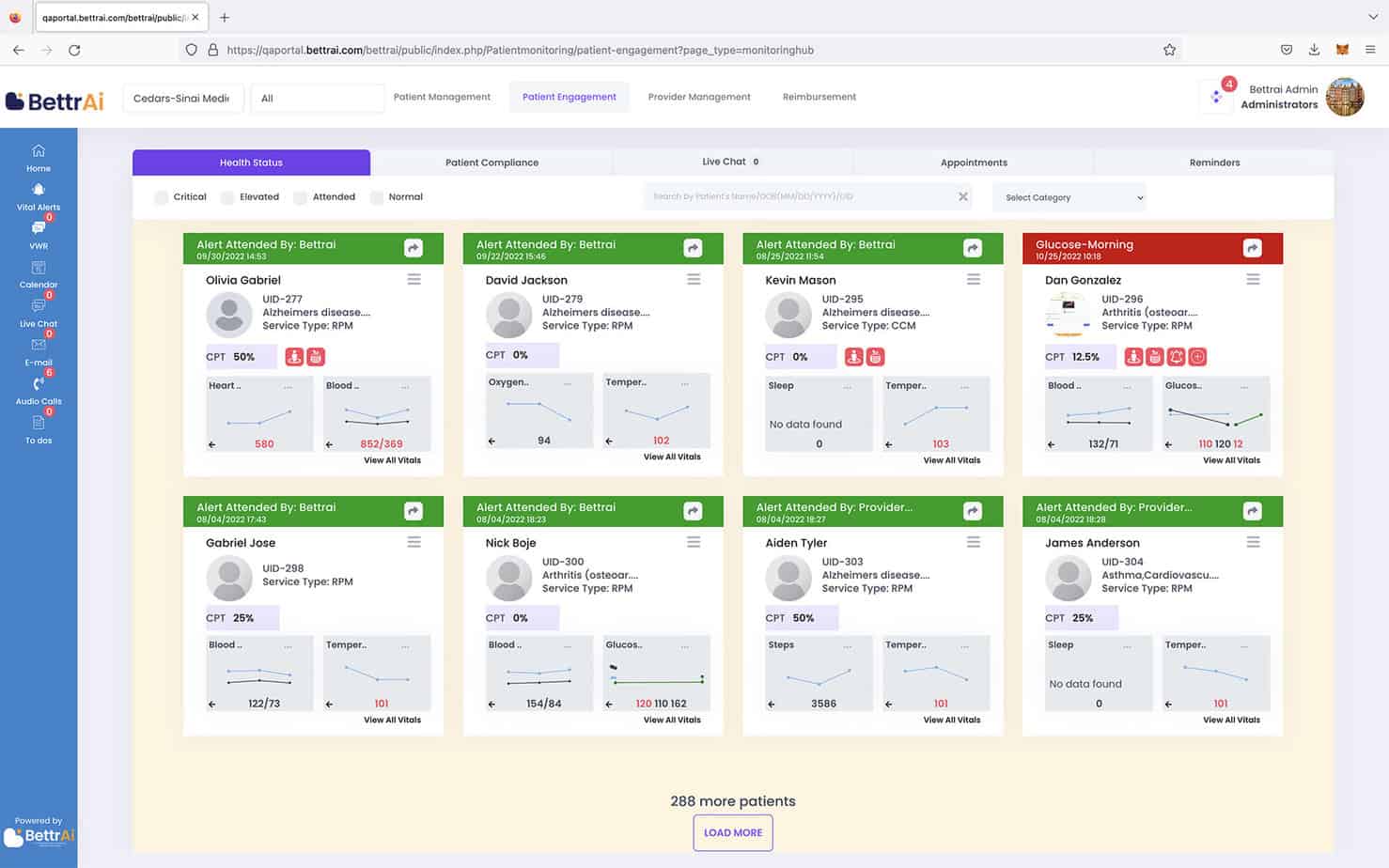
The BettrAi platform harnesses the power of Artificial Intelligence to enable
- advanced analytics of big data for entire cohorts of patients
- real-time trend analysis
- customizable predictive models
Provider organizations become capable of managing care of individual patients and their entire patient population in real time, allowing them to deliver the right care at the right time and in the most appropriate setting.
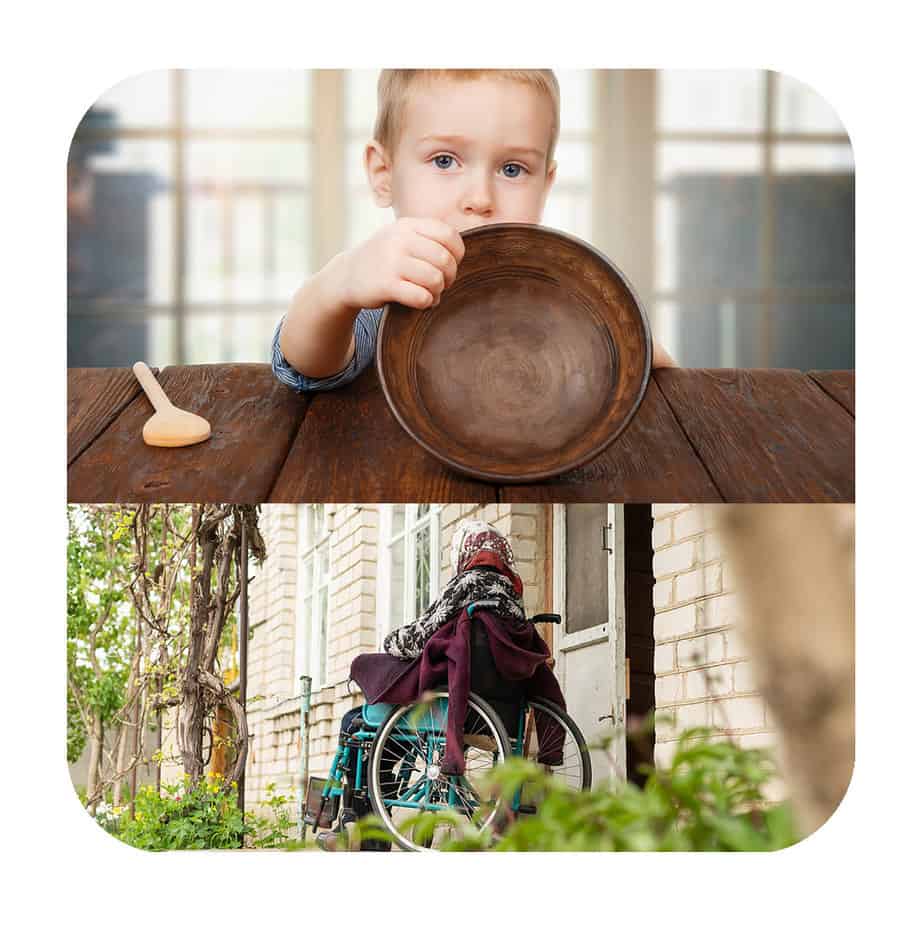
With approximately 50% of the U.S. population suffering from at least one chronic condition and accounting for nearly 90% of healthcare expenditures, we can and we must do better at preventing the adverse health events which frequently result in ER visits, hospitalizations, readmissions, and unnecessary morbidity and suffering.
BettrAi’s comprehensive set of dashboards display individual patient profiles containing both current and historical clinical data and trends over time: medications, allergies, immunizations, screenings, lifestyle habits, current health issues, vital signs including weight, BMI, temperature, heart rate, blood pressure, and where applicable, pO2, blood glucose, and other measures.
Social Determinants of Health (SDoH) are likewise captured and built into predictive models that enable providers to manage risk proactively, rather than reactively.
Food, housing, and transportation insecurity can massively impact a patient’s prognosis and likelihood of an adverse event. Social supports, economic security, and educational status further impact one’s level of risk. The SDoH, once regarded as somewhat tangential, or at least secondary, to a patient’s likely disease course, and thus, generally relegated to another “silo” of responsibility, are instead, now understood to be absolutely central to the patient’s healing, recovery, and stabilization.